By Dr. Darko Stamenkovski
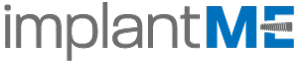
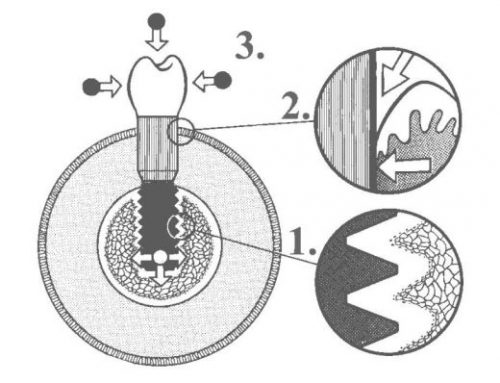
The goal of modern implant therapy entails more than just the successful osseointegration of the implant. A successful result must also include an esthetic and functional restoration surrounded by stable peri-implant tissue levels that are in harmony with the existing dentition. In an attempt to improve long-term bone maintenance around implants, a new implant-to abutment connection referred to as “platform switching” has been proposed. It refers to the use of an abutment of smaller diameter connected to an implant neck of larger diameter.
In 1991, 3i Implant Innovations (BIOMET 3i Inc., FL) aimed to construct wide-diameter implants with the larger diameter restorative platforms than standard implants. But, for some time, corresponding prosthetic components were unavailable; hence, standard prosthetic abutments (4.1 mm diameter) were used instead of abutments that matched the 5 and 6 mm implant diameters. The consequence of this form of treatment was an unintentional “change of platform”, which became known as platform switching (PLS).
After a 5-year period, the typical pattern of crestal bone resorption was not observed in platform switched implants. Thus, the discovery of the concept was a coincidence.
Clinical relevance of platform switching
-Increased biomechanical support – Where anatomic structures such as the sinus cavity, the nasal floor, the incisive canal, and the alveolar nerve limit the residual bone height
-Effect on soft tissue esthetics around dental implants – Tarnow et al. showed how the presence of the gingival papilla is influenced by the distance between the implants. When two implants are placed close to one another (inter-implant distance 3mm or less) the inter-implant bone height can resorb below the implant-abutment connection, reducing the presence of an inter-implant papilla. This may affect the clinical result in the esthetic zone. Platform switching reduces this physiologic resorption by moving the microgap away from the inter-implant bone that supports the papilla. This helps to avoid cosmetic deformities, phonetic problems and lateral food impaction.
The dynamics involved when an implant is placed are now understood. The crestal bone changes that occur can have a profound effect on treatment outcome and will influence implant location, design, and manufacturer. In addition, restorative options for osseointegrated implants will be greatly influenced by these crestal bone changes. Platform switching is a way in which the harmful effects of bone remodeling can be decreased and help to ascertain a more predictable outcome thereby improving esthetic expectations.
Platform switching configuration has the biomechanical advantage of shifting the stress concentration area away from the cervical bone–implant interface. It also has the disadvantage of increasing stress in the abutment or abutment screw.
Many factors contribute to marginal bone loss around implants and its solution cannot be attributed to any single parameter. However, an appropriate understanding and use of platform switching concept in routine treatment improves crestal bone preservation and controlled biologic space repositioning. It appears be a promising tool in preserving peri-implant bone and further research is needed to substantiate its application in contemporary implantology.
READ MORE:
http://www.joponline.org/doi/abs/10.1902/jop.2010.100232
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808029/
http://www.ncbi.nlm.nih.gov/pubmed/16013682/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309512/