Bioengineering is critical in dental implant biodesign. Design means to create according to a plan.The word design indicates a process, not an end product. Design has some identifying characteristics. A complicated design problem will usually be broken down into sub-problems, so these can be addressed separately and then considered together in reaching final solutions. Often, design must go forward even when there is missing or unknown information. In design, judgments about the quality of a solution are made by measuring performance against the stated goals, not the other way around.
Finally, design is often iterative. There may be a need to design and redesign several times to optimize performance with respect to goals. There may be no perfect solution to a design problem, but instead a compromise solution representing the best solution under conflicting constraints.
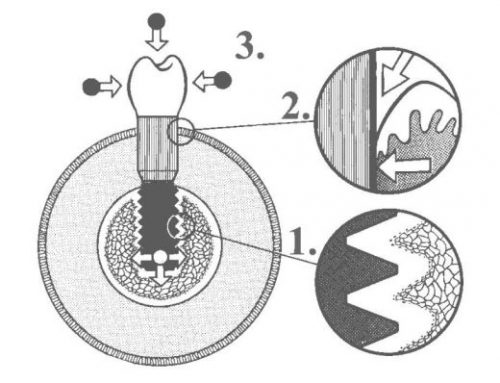
Modern implants consist of an osseous part that interacts with the bone, a transmucosal component that interacts with the mucosa and then the restoration; this can be a crown or bridge abutment, or anchors for dentures.
In recent years,there has been a vast amount of scientific development in implant design, geometry, materials and techniques in order to improve the ease of delivery and success of implant treatment.
The majority of designs are cylindrical, or rootform in geometry. Also implants can be “tapered” or “parallel sided” in profile and almost exclusively
endosseus, i.e. placed within the alveolar bone rather than subperiosteally or intramucosally. Surfaces are normally roughened (microporous) through use of surface preparation (e.g.sand blasting and acid etching) rather than being coated to increase the surface area available for osseointegration
Majority of modern root form dental implants are “threaded” in design although the thread pitch or profile can vary significantly between manufacturers.
Micro-threaded implants employ small threads around the neck of the implant to engage the dense cortical bone better and to distribute occlusal loads more optimally. This has been shown to reduce the shrinkage of the crestal bone through enhanced biomechanical fixation and loading. Other implants use different thread designs to improve their stability, particularly in softer bone.
Implant surfaces also show variations. Surface hydrophilicity enhances adherence of biomolecules and promotes the initiation of the osseointegration
process. Almost all modern implants today have a microporous (rough) surface rather than a relatively smooth machined surface. Roughness increases the surface area available for more “bone-implant contact”.
Some implant surfaces are treated with bioactive substances such as fluoride to enhance the process of osseointegration. One implant system uses laser etching to promote adherence of hard and soft tissues to the shoulder portion of the implant as it emerges from the crestal bone. It has been suggested that this can help to resist apical migration of the peri-implant tissues.
Macroscopically, an implant may or may not have a polished collar that protrudes above the crestal bone into the soft tissues. Implants that are
fully inserted within the alveolar bone are known as “bone-level implants”. Restorative components are designed to fit on top of the implant (external
connection) or within the implant (internal connection). If an abutment larger in diameter than the diameter of the implant is used – this is known as “platform switching” which has been shown to offer distinct mechanical and biological advantages.
Different implant designs and procedures are being introduced constantly as implantology continues to evolve. These new products have been subject to varying levels of research and development and clinical documentation with the implications that some materials or procedures may prove to be less reliable or safe in routine use. Since clinicians are bound by ethical and medicolegal responsibilities, the onus is very much on the treating dentist to select the most appropriate procedure or material depending on individual circumstances.