By Prim. Dr. Tome Tasevski
Implant treatment in individuals with periodontitis-associated tooth loss is frequently debated, because dental implants have become widely recognized as a treatment modality in patients with tooth loss. As an increasing number of patients receive implant therapy to replace missing teeth due to periodontal disease, the question arises as to whether the outcome of dental implants is influenced by a history of periodontitis.
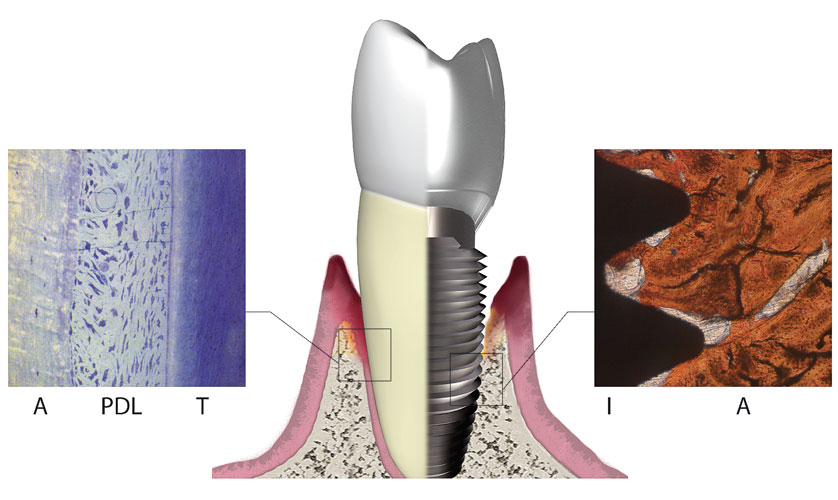
Periodontitis comprises a variety of pathologic conditions that affect the health of the periodontium and is commonly seen in its chronic form. In general, patients exhibit gingival inflammation with destruction of tooth-supporting structures including the periodontal ligament, connective tissue, and bone. Aggressive periodontitis forms are characterized by rapid attachment loss and alveolar bone destruction in otherwise systemically healthy individuals.
This patient population is believed to carry an increased risk for implant failure, increased probing depths, and progressive bone loss around implants. Because inflammatory periodontal disease is regarded as a leading cause of tooth loss in the adult population, the issue in regards to successful implant placement becomes a major consideration for the clinician in treatment planning patients with a history of periodontal disease.
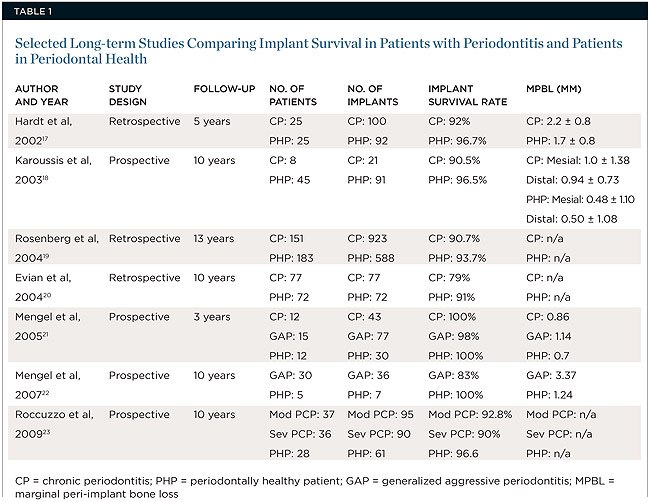
Numerous long-term studies have been conducted on this topic:
A 10-year prospective study conducted by Karoussis et al found that, although patients with a previous history of periodontal disease had a significantly higher incidence of peri-implantitis (28.6% vs. 5.8%) than their healthy counterparts, implant survival rates were still clinically favorable, with results of 90.5% seen in patients with a past history of chronic periodontitis compared to 96.5% in periodontal healthy subjects.
Implant placement in patients with a history of generalized aggressive periodontitis (GAgP) might be considered a viable option to restore oral function with survival outcomes similar to those found in both patients with chronic periodontitis(CP) and healthy patients (HP). However, the risk ratio for failure in patients with GAgP is significantly higher when compared with HPs and those with CP.
A total of six non-randomized prospective clinical trials met the inclusion criteria. The results showed survival rates of 83.3% to 100% (GAgP), 96.4% to 100% (CP), and 96.9% to 100% over a mean period of 48.01 ± 71.99 months (Alberto Monje et al )
The literature currently indicates no significant difference in the rate of implant survival between patients with a history of periodontitis and periodontal healthy individuals after 5-year follow-up; however, studies show that patients with a history of periodontitis manifest greater probing depths, more marginal bone loss surrounding implants, and a higher incidence of peri-implantitis. With carefully monitored supportive periodontal therapy (SPT) and proper management, clinical studies show implant survival at 5- and 10-year follow-up to prove dental implants to be a successful treatment modality with a predictable outcome.
Supportive periodontal therapy, defined as regular visits to the clinician for periodontal control and maintenance, formed the basis of long-term success after periodontal implant placement. SPT was shown to be an effective method in maintaining implant success and preventing periodontitis recurrence. All patients revealed improvement in plaque control, with statistically significant differences between initial plaque scores and 10-year follow-up values. Patients with chronic periodontitis who did not completely adhere to SPT demonstrated a higher incidence of implant loss. (Roccuzzo et al.)
Prophylactic antibiotics are frequently administered prior to placement of implants to minimize the risk of infection. Amoxicillin is commonly prescribed pre- and postoperatively in addition to a chlorhexidine rinse
Patients with a history of periodontal disease should be informed that there is a higher risk of peri-implant disease. The survival of dental implants in this population was not significantly different from periodontally healthy patients. However, patients with a history of periodontitis demonstrate a significantly higher frequency of peri-implantitis and peri-implant bone loss. Supportive periodontal therapy seems to be a key factor in enhancing long-term implant survival.
With proper management and patient compliance, the literature suggests that clinically acceptable results can be achieved when placing dental implants in patients with a history of periodontitis. However, there is a need for stronger evidence in the form of longitudinal studies in much larger samples in the future.
READ MORE:
http://onlinelibrary.wiley.com/doi/10.1034/j.1600-0501.000.00934.x/full
http://www.ncbi.nlm.nih.gov/pubmed/18181930
http://www.joponline.org/doi/abs/10.1902/jop.2005.76.4.534
http://onlinelibrary.wiley.com/doi/10.1034/j.1600-0501.1992.030303.x/full
http://www.tandfonline.com/doi/full/10.4161/21505594.2014.980661
http://www.joponline.org/doi/abs/10.1902/jop.2013.130088
http://www.joponline.org/doi/abs/10.1902/jop.2014.140135